Cardiac Ultrasound
Background
Cardiac ultrasound is an essential tool for Anesthesiologists with uses in all phases of the perioperative period. Preoperatively, cardiac POCUS can be used to risk-stratify patients and assess for pathology. Beyond this, cardiac ultrasound is a useful perioperative adjunct for shock assessment, volume status evaluation and investigating ischemic symptoms or ECG changes. With the increased availability of ultrasound equipment and the incorporation of TTE education into most anesthesia residency programs, competency in basic cardiac ultrasound is an expectation.
Indication
-
Shock/volume assessment
-
Syncope/presyncope
-
Shortness of breath
-
ECG findings/ischemic symptoms
-
Murmurs
-
Cardiac arrest
-
Preoperative assessment of LV function/valvular lesions
Acquisition
Transducer: Phased array
Patient Position:
-
Supine
-
Left lateral decubitus if supine views suboptimal
Operator Mechanics
-
Operate probe with dominant hand
-
Place ultrasound machine on same side as operator to manipulate controls with non-dominant hand
-
This may mean that right-handed operators are reaching over to patient’s left side
Scanning Technique
-
Ensure ultrasound machine set to the cardiac preset: on-screen indicator should be to the RIGHT of the image
-
Begin scan with patient in supine position
Parasternal Long Axis (PLAX)
-
Place probe over the third or fourth intercostal space just to the left of the sternum
-
The indicator light is directed towards patient’s right shoulder
-
Scan between rib spaces in order to find an acceptable view of the heart structures
-
At this level, the left ventricle should be visualized to appear as long as possible
-
The LA, LV, LVOT and a small bit of the RV will be visualized
-
The AV and MV will be visualized




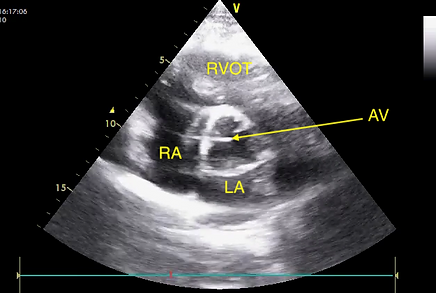
Parasternal Short Axis (PSAX)
-
From parasternal long axis view, rotate probe clockwise 90º so that indicator light is directed to patient’s left shoulder
-
PSAX - Aortic Valve
-
To find this level, slide the transducer cranially (towards the right shoulder), along the axis of the heart and identify the characteristic “Mercedes-Benz” appearance of the aortic valve
-
The three cusps of the aortic valve are seen centred on the screen
-
The right coronary artery is often visualized
-
-
As opposed to the other short axis views, the base level can visualize the LA, RA, tricuspid valve, RV and RVOT
-

-
PSAX - Mitral Valve
-
To find this level, tilt the transducer towards the apex (away from the right shoulder), along the axis of the heart and identify the characteristic “fish-mouth” appearance of the mitral valve
-
The anterior and posterior leaflets of the mitral valve are seen centred on the screen
-
This view is mostly used to assess the mitral valve, but the LVOT and RV are also visualized
-


-
PSAX - Mid-Papillary
-
To find this level, slide the transducer caudally (away from the right shoulder), along the axis of the heart and identify the papillary muscles, which appear as paired mobile structures at the deep side of the screen
-
The anteroloateral and posteromedial papillary muscles will be seen
-
The mid-papillary view enables a good estimation of LV function, size and wall thickness
-
The interventricular septum and RV are also visualized
-
Normal septal motion: septum goes inwards toward the LV cavity during systole
-
-


-
If concerned about any regional wall motion abnormalities, can scan the entirety of the LV from base to apex
-
PSAX - Apex


Apical Four-Chamber (A4C)
-
The apical four-chamber view is likely the highest-yield view in terms of global assessment of cardiac function and number of structures visualized
-
Place probe over the fifth or sixth left intercostal space at the midclavicular line with the indicator light directed towards patient’s left side at the 3 o'clock position
-
This often coincides with the point of maximal impulse
-
Alternatively the A4C view can be obtained by sliding the probe in the PSAX view to the apex, then tilting the transducer towards the base (towards the right shoulder)
-
-
The LA, LV, RA and RV should be clearly identified
-
The MV and TV are well viewed at the A4C window
-
Variations of the A4C include the apical two-chamber, three-chamber, five chamber and coronary sinus views



Subcostal Four-Chamber (S4C)
-
The subcostal four-chamber view is the best global cardiac view when the A4C is particularly challenging (e.g. obstructive lung disease)
-
The S4C assessment is used in eFAST and is often the best view for identifying pericardial effusions
-
Place probe beneath the xiphoid process, with the face of the ultrasound directed towards the patient’s left shoulder
-
Often requires some degree of posterior pressure
-
May require the patient's knees to be bent and head slightly elevated to improve view
-
-
-
The indicator light is directed towards patient’s left side at the 3 o'clock position
-
Structures visualized are similar to the A4C view
-
From the S4C view, it is relatively easy to assess the IVC (described in the IVC module), and this assessment should be part of a holistic cardiac assessment



Interpretation
** Qualitative assessments should be based on multiple views and cuts
Left Ventricular Assessment
-
LV ejection fraction
-
Qualitative
-
Inward motion of the ventricular walls
-
Motion of the mitral annulus
-
-
Quantitative
-
Simpson method
-
Fractional shortening
-
-
-
LV size
-
Normal
-
Reduced
-
Enlarged
-
-
LV wall thickness
Right Ventricular Assessment
-
RV ejection fraction
-
Qualitative
-
Quantitative
-
TAPSE
-
-
-
RV size
-
Normal
-
Reduced
-
Enlarged
-
Aortic Valve
-
Number of leaflets
-
Leaflet thickness
-
Valve motion
-
Restriction
-
Prolapse
-
-
Regurgitation
-
Colour doppler
-
Mitral Valve
-
Leaflet thickness
-
Valve motion
-
Restriction
-
Prolapse
-
-
Regurgitation
-
Colour doppler
-
Assessment for Pulmonary Embolism
-
Obstruction of the pulmonary vessels with emboli lead to pressure overload, which can have distinct TTE manifestations
-
RV pressure load can lead to an “RV strain pattern”, which appears as a dilated RV with reduced systolic function
-
LV usually has normal systolic function, but is more collapsed in a characteristic “D-shape” from RV overload
-
This is best seen in the PSAX view
-
-
McConnel’s sign: akinesia of RV mid free-wall with normal motion at the apex
-
Very specific for PE
-
Pericardial Effusions
-
Best visualized in the subcostal and PLAX views
-
Tamponade is compression of the heart from a pericardial effusion
-
Typically see RA systolic collapse followed by RV diastolic collapse
-
Medical Decision Making
Preoperatively
-
Delay case for medical optimization/formal TTE
-
Alter anesthetic plan based on findings
-
Determine baseline cardiac function
Intraoperatively
-
Investigate impact of anesthetic medications on cardiac function
Postoperatively
-
Evaluate etiologies of shock and hypoxemia to guide fluid resuscitation and treatment
-
Pursue more aggressive imaging modalities to evaluate post-op pathology
Pitfalls and Modifications
-
If encountering difficulty with image acquisition, ask the patient to turn towards the left lateral decubitus position and raise their left arm above their head to bring the heart closer to the chest wall and expand the space between ribs
-
Lung disease: hyperinflation can make parasternal and apical views challenging to obtain
-
Typically still able to acquire subcostal views
-
-
Qualitative assessments of non-binary parameters (i.e. LVEF) can lend themselves to over and underestimation
-
Very important to assess cardiac function with all views
Comprehension Questions
1. Which cardiac view is used in eFAST and is best for identifying pericardial effusions?
A. Subcostal Four-Chamber
B. Apical Four-Chamber
C. Parasternal Long
D. Parasternal Short
2. Which view is the highest yield for assessing global cardiac function?
A. Subcostal Four-Chamber
B. Apical Four-Chamber
C. Parasternal Long
D. Parasternal Short
3. What are two characteristic findings on TTE with pulmonary embolism?
4. Which view should be obtained to evaluate LV ejection?
A. Subcostal Four-Chamber
B. Apical Four-Chamber
C. Parasternal Long
D. Parasternal Short
E. All of the above
5. Which view should be obtained to evaluate the mitral valve?
A. Subcostal Four-Chamber
B. Apical Four-Chamber
C. Parasternal Long
D. Parasternal Short
E. All of the above
Answers
1. A
2. B
3. Dilated RV and D-shaped LV
4. E
5. E
References
Binder, T. (2018, September 6). 123sonography echo e-book. 123 Sonography. Retrieved May 5, 2022, from https://123sonography.com/ebook
Cativo Calderon, E. H., Mene-Afejuku, T. O., Valvani, R., Cativo, D. P., Tripathi, D., Reyes, H. A., & Mushiyev, S. (2017). D-shaped left ventricle, anatomic, and physiologic implications. Case Reports in Cardiology, 2017, 1–4. https://doi.org/10.1155/2017/4309165
Foster, E., & Manning, W. J. (2022). Echocardiographic evaluation of the aortic valve. In UpToDate. Retrieved May 1, 2022, from https://www.uptodate.com/contents/echocardiographic-evaluation-of-the-aortic-valve.
Li, V., & Dinh, V. (n.d.). Cardiac Ultrasound (echocardiography) made easy: Step-by-step guide. POCUS 101. Retrieved May 1, 2022, from https://www.pocus101.com/cardiac-ultrasound-echocardiography-made-easy-step-by-step-guide
Melgarejo, S., Schaub, A., & Noble, V. E. (2017, October 31). Point of care ultrasound: An overview. American College of Cardiology. Retrieved May 5, 2022, from https://www.acc.org/latest-in-cardiology/articles/2017/10/31/09/57/point-of-care-ultrasound
Patel, A. R., & Shefner, J. (2020). Transthoracic echocardiography: Normal cardiac anatomy and tomographic views. In UpToDate. Retrieved May 1, 2022, from https://www.uptodate.com/contents/transthoracic-echocardiography-normal-cardiac-anatomy-and-tomographic-views
Schiller, N. B., Ren, X., Ristow, B., & Manning, W. J. (2022). Echocardiographic evaluation of the mitral valve. In UpToDate. Retrieved May 1, 2022, from https://www.uptodate.com/contents/echocardiographic-evaluation-of-the-mitral-valve.
