IVC Ultrasound
Background
Ultrasound-guided volume assessment is a frequently used tool in the perioperative setting. Despite some concerns about the utility of inferior vena cava assessment, a comprehensive volume exam including IVC assessment and focused cardiac ultrasound can provide some useful information, especially when patients are on the extremes of volume status (overloaded or in shock). Combining volume assessment with lung ultrasound and other monitoring (i.e. SPV and PPV) can help guide fluid management.
Indication
-
Shock NYD
-
Guided fluid resuscitation
-
Dyspnea NYD
Acquisition
Transducer
-
Phased array
-
Curvilinear low frequency
Patient Position:
-
Supine
-
Left lateral decubitus if supine views suboptimal
Operator Mechanics
-
Operate probe with dominant hand
-
Place ultrasound machine on same side as operator to manipulate controls with non-dominant hand
Scanning Technique
-
Easiest to begin examination after focused cardiac ultrasound (see module)
-
From subcostal view, while visualizing the right atrium, locate the IVC in center of the liver
-
Rotate probe keeping the IVC in the centre of the screen so that the indicator is pointed caudad
-
Fan back and forth to ensure you are viewing the maximal diameter of the IVC
-
-
Size: measure maximal diameter of the IVC
-
The point of maximal diameter is often at the junction of the IVC and RA or 1-2 cm caudal to the junction
-
-
Respirophasic variation
-
Put the ultrasound into M-Mode
-
Place the caliper perpendicular to the IVC at either measurement site
-
Ask patient to take a deep breath or sniff through their nose
-
Measure the maximum and minimum diameter of the IVC
-
-
Important to perform follow-up scans to evaluate any changes that occur with interventions



Interpretation
-
There is a fair bit of controversy on the utility of IVC assessment
-
It's important to ensure that other things that increase CVP are not present (i.e. obstructive shock, right heart failure, elevated intrathoracic pressure)
-
The following table is an adaptation from a review of the evidence by Dr. Justin Bowra at the SMACC Conference:

Medical Decision Making
-
Hypovolemia
-
May indicate possibility of occult bleeding
-
May guide fluid administration and efficacy of intervention
-
-
Hypervolemia
-
In conjunction with lung ultrasound, may guide diuresis
-
In context of hypotension, suggests that fluid administration will not be helpful
-
Pitfalls and Modifications
Aorta
-
Ensure that the IVC is viewed at maximal diameter to avoid falsely low values
-
Ensure visualization of IVC draining into RA to avoid measuring the aorta
-
The IVC is simply an estimation of the CVP and is subject to the same issues with interpreting CVP
-
Assessment of the IVC should be paired with a focused cardiac and lung ultrasound assessment
Comprehension Questions
1. In a spontaneously breathing patient, which collapsibility percentage correlates with fluid responsiveness?
A. > 10%
B. > 20%
C. > 40%
D. > 60%
E. > 80%
2. In a mechanically ventilated patient, which collapsibility percentage correlates with fluid responsiveness?
A. > 5%
B. > 8%
C. > 18%
D. > 30%
E. > 60%
3. Which standard ultrasound view is optimal for visualizing the IVC?
A. Apical Four-Chamber
B. Subcostal Four-Chamber
C. Parasternal Long-Axis
D. Parasternal Short-Axis
4. Of the following, which condition does NOT lead to a distended IVC?
A. Hypovolemia
B. Pulmonary embolism
C. Hypervolemia
D. Pulmonary hypertension
E. Right heart failure
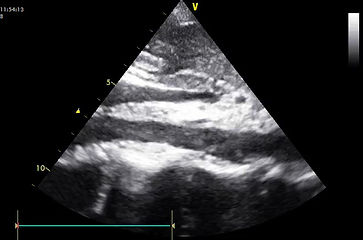
5. Label the following: right atrium, right ventricle, IVC, hepatic vein, liver
Answers
1. C
2. C
3. B
4. A
5.


References
Bowra, J. (2013, July 7). IVC Ultrasound: The Ultimate Myth. Lecture presented at SMACC in Australia, Sydney.
Bowra, J. (n.d.). CCUS Manual 3: Scanning the IVC. In The San Critical Care Ultrasound Manual. Retrieved May 1, 2022, from https://aci.health.nsw.gov.au/networks/eci/clinical/clinical-tools/ultrasound-in-the-ed/ultrasound-critical-care.
Corl, K. A., George, N. R., Romanoff, J., Levinson, A. T., Chheng, D. B., Merchant, R. C., Levy, M. M., & Napoli, A. M. (2017). Inferior vena cava collapsibility detects fluid responsiveness among spontaneously breathing critically-ill patients. Journal of Critical Care, 41, 130–137. https://doi.org/10.1016/j.jcrc.2017.05.008
Dinh, V., Cardiac Ultrasound (Echocardiography) Made Easy: Step-By-Step Guide. Retrieved from https://www.pocus101.com/cardiac-ultrasound-echocardiography-made-easy-step-by-step-guide/
Eggeman, D., Ghaffarian, K., Camilon, M., Y., Young, N., Ostermayer, D., . . . Ye, T. (2020, August 20). IVC ultrasound. Retrieved from https://wikem.org/wiki/IVC_ultrasound
